 Ok let’s face it, any surgical operation has its inherent risks and problems. And the same can be said about dental implant operation.
Ok let’s face it, any surgical operation has its inherent risks and problems. And the same can be said about dental implant operation.
But before diving into the main dental implant problems, if you don’t know much about implants, I advise you to read our 101 guide on dental implants, so everything that follows will make sense. It covers the basics and will only take you a few minutes to read.
For most cases, dental implants are a no-brainer choice when it comes to replacing a missing tooth or teeth, by using implants as roots to anchor teeth into the jawbone.
The average sucess rate is pretty impressive, which is about 95%. It can even go as high as 98% with some very experienced and skilled dentists.
By the way, if your dentist assures you implants are 100% successful, then alarm bells should start to ring, and you should probably seek another dentist.
In fact, there is 5 or 2% failure that you must be aware of.
Most of those failures are caused by bad planning or uncomplete assessment of the patient’s bone conditions, which is often associated with a lack of skills or inexperienced dentists. But fortunately, most issues can be easily solved if corrrective actions are taken quickly.
I know that no one wants to know or hear about those complications but when taking a decision, you need to see the whole picture with the pros and the cons. That is the wisest way to to go.
Besides, the more you know about possible complications, the more you can help monitor the evolution of your implants and alert your dentist if you notice something wrong. That is the best way to avoid further complications.
Implant is loose or is falling out
This is probably the main dental implant problems. This happens when the bone does not grow and fuse with the implant (between the threads of the implant).
This is what we call the osseointegration failure. You know by now, osseointegration is the process by which the dental implant material fuses with the bone. This process is usually completed within a few months, resulting in a strong and tight connection between the implant and the jawbone. So, the implant is tightly fixed to the jawbone and won’t move when chewing.
If this process does not occur correctly, your dental implant will not function properly. It will become uncomfortable, become loose, or fall out completely.
Bone loss after the implant is placed, is also another indicator. Bone loss of less than 0,2 millimeter a year after the operation is tolerable; more than that, it would be considered a failure.
Keep in mind some slight bone loss over many years is normal, which can be considered normal age-related bone loss, but it shouldn’t affect your implants directly.
What are the main reasons of failed ossointegration?
- Inaccurate positioning: a faulty alignment of the implant can lead to forces that can prevent the bone to sucessfuly grow around it.
- Excessive loading or overloading: the functional load applied to the implant exceeds the capacity of the bone to support it and affects the bone growing.
- Volume or density insufficiency of the bone
- Damage to the tissue surrounding the implant
- Oral or intravenous bisphosphonates (fosamax, actonel or boniva) that can affect the ability of the jawbone to heal
- Blunt force trauma that affects the healing and bone integration process
- Formation of a thin fibrous capsule around the implant
- Dental implant Inflammation
- Infection
If osseointegration does not take place, the dental implant can be removed, and surgery can be attempted again once the implant area has fully healed.
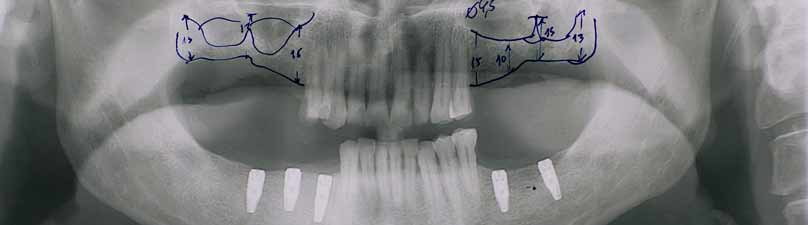
This illustrates why the assessment of your jawbone is certainly the most important part of the procedure because if your dentist tries to place implants in a « weak » jawbone, then you can expect a higher rate of failure.
Prior to the operation, the dental specialist must first establish the integrity of your jawbone to support the implant. Measurements of your bone’s height, width, and density are taken to make sure that it can hold the implant in place.
If necessary, procedures like bone grafting or sinus lift (a bone grafting in the sinus area) will be required to ensure that you have a solid bone mass that will support osseointegration.
Overloading : when impatience leads to dental implant problems
Overloading has been listed above as a failed ossointegration cause; I wanted to give you a little more details about this issue.
So what is it? Overloading is a result of applying severe pressure on the area of dental implant operation. This is most commonly observed in implants where the implant (the post or the screw part) and the abutment are placed at the same time. (Remember the 3 stages of a dental implant operation?)
On this procedure, the abutment protrudes out of the gum while the implant is still in the process of osseointegration. So it means extra care is needed when you opt for this procedure because any pressure exerted on the abutment during the healing process will cause further injury and may actually prevent full integration of the bone and the implant. That means a bad ossointegration and a loose implant as a result.
If you are sure that you will be able to take good care of your implant, this all-in-one procedure may save you a lot of time because you will have 2 procedures done in one operation.
But if you consider long-term safety and benefits, you’d better be on the safe side by undergoing a 3-stage dental implant procedure where the implant (post or screw part) is placed first. You would wait for 3-4 months for the bone to fuse with the implant, then the dentist would set up the abutment and then the crown. It is a bit longer but it is worth sometimes to wait longer for a more successful implant surgery.
Fosamax, actonel, boniva : possible complications with biphosphonates
You know dental implants need to be fully integrated to the jawbone to be considered a success, so as you can imagine any medication that affects the bone healing process, might be an issue to get these implants perfectly embedded in the bone.
Still not clear?
Fosamax, actonel and boniva are famous medications called biphosphonates that have been widely used for the prevention and treatment of osteoporosis (a bone disease associated with a decrease in bone mass and density leading to an increased risk of fracture)
These drugs actually prevent bone from breaking down so as a net result the bone density or thickness increases.
But then what is the problem? When you have dental implants, the dentist will make holes to insert the implants, so he or she will kind of break your bones. These bones will have to grow into the implant. Yet bone healing is a complex process that involves breaking (or resorbing) and bone forming, it is more of a bone remodeling process. So because biphosphonates inhibit the bone resorbption phase, these medications will prevent the bone to heal normally and lead to what dentists call jaw osteonecrosis.
What is jaw osteonecrosis? This is a destructive process of the jawbone, with the bone being exposed in the mouth and the gum doesn’t heal over it.
So what are your options?
Well there are 2 cases:
- If you take biphosphonates intravenously, then the dental implant procedure is more at risk, so it is in most cases contraindicated
- If you take them orally, then you have more chances to get implants. Yet, the risk of osteonecrosis is less high depending on the treatment duration. The longer the treatment prior to the considered implant operation, the higher the risk. If you have taken oral biphosphantes for less than 3 years, then the risk is lower.
Whatever your personal situation, please keep in mind nothing is all black or white and some dentist have had great results even with patients with biphosphonates treatment. Nothing is set in stone. Let simply your dentist check your risk and give you his or her personal opinion on your rate of success.
This also highlights the importance of giving your complete medical and dental history, so your dentist gets all the elements to better assess your risks.
Implant Infection or Peri-implantitis
Dental implant infection is also called peri-implantitis.
What is it? It is an infectious disease leading to inflammation of the surrounding gum and bone of a dental implant, causing the loss of supporting bone.
How? Inflammation triggers an inflammatory response from the body’s immune system that can attack gum tissues and surrounding bone. This can lead to bone loss around the dental implant, which will make the implant loose in the long run if untreated.
It can be contracted when bacteria is present during the different stages of dental implant operation or at any time after the surgery if proper dental hygiene is not observed, leading to bacteria growth. This can happen due to non-sterile technique, a contaminated implant and pre-existing infection that was not treated.
In the early stages, this condition usually evolves silently without the patient noticing the bone loss around the dental implant.
Peri-implantitis can happen several months or years after the surgery and is reported to be more frequent among people who:
- Smoke: smoking reduces dental implant success rate because it causes constriction of blood vessels, which limits the bone growth, leading to bone loss as a net effect. So, quitting smoking would be highly advised prior the operation. Good motivation factor, isn’it?
- Suffer from diabetes: diabetes make patients more susceptible to infection, slows down normal healing, and is also associated with several vascular diseases. These conditions can increase the risk of complications following surgery of any kind. This is mainly the case with uncontrolled diabetes. On the other hand, if the patient is compliant with his or her diabetes medication and do manage to control his/her level of blood sugar, then the rate of success is much higher, which explains the good results some dentists have even with diabetic patients.
- Have poor immune systems that won’t be able to cope with oral infections.
- Have thin gums that easily expose the bone underneath to decay or infection, which may be solved with some gum grafting.
- Have very poor dental hygiene, which leads to bacteria growth. You know what to do here: brushing twice a day (or 3 times after each meal) for 2-5 minutes minimum.
Note: if too much cement is used to fix the crown on the implant, the extra cement can also get down near the gum and lead to a gum inflammation. That’s why many crowns are held in by screws rather than with cement.
What are the peri-implantitis symptoms?
Please note they don’t necessarily appear at once in the early stages of the infection, that’s why you need to urgently contact your dentist when you notice them to prevent further complications.
- Abnormal bleeding at the gumline
- Gum looking very red, or a bit purple/ blue (gum irritation or inflammation)
- Pus coming out from the gum near the implant, which will lead to a bad mouthtaste
How to treat it?
Your dentist will try to stop the bone loss and save the dental implant by prescribing antibiotics and cleaning the implant area thouroughly with antibacterials such as iodine.
However, because most patients don’t notice the bone loss or the infection right from the start, the above procedure won’t probably be enough and most cases will require antibiotics, surgery and bone grafting.
The dentist will reopen your gums to clean the area and will need to graft some bone (human, cow, your own bone or synthetic), with the hope the bone graft will fuse around the implant. Of course the more bone loss, the lower the success rate.
Severe peri-implantitis cases will then require the removal of the dental implant; bone grafting to fill in the hole and placing a new implant once the area has fully healed
Damage to Nerves and Tissues
These damages to surrounding tissues or nerves are mainly due to the inexperience of the dentist. An experienced and skilled impant expert is able to identify any potential issues by checking the x –rays or CT scans and can minimize these risks.
What could be damaged?
– surrounding teeth : the dentist can damage the root of an adjacent teeth when drilling into the jawbone. All of us don’t have perfect aligned teeth, that’s why the dentist must review carefully the position of the other teeth (and roots) before drilling. That is all part of the planning.
– nerve damage : this can happen when the implant surgery takes place in the lower jaw. There is a nerve called inferior alveolar nerve that runs trough the lower jawbone. The damage can occur because the implant is placed too close to this nerve running through the gums or if the nerve is hit during the operation. What are the signs of nerve damage? Patients feel pain, numbness, or tingling sensation in their gums and facial areas near the location of the implant such as cheek, chin, lips, or tongue. The damage to the nerve may be permanent or temporary, but there might be a need to extract the implant in most cases. X-rays and CT scans help the dentist to identify the exact location of the nerve and minimize the possibility of nerve damage.
– Perforation into sinus: our face bones are hollow and do contain air spaces called sinuses. The sinuses above the upper back teeth are called maxillary sinuses. So the sinus perforation can happen when the implant surgery takes place in the upper jaw. What are the signs ? Some patients felt some pressure or had a stuffy nose, the risk is mainly the possibility of a bad sinus infection, so the implant may have to be removed, so you can get this area properly repaired before placing a new implant. Usually a CT scan will help to check if the sinus has been perforated.
To prevent this complication, a sinus lift is often necessary prior to the dental implant placement. It means increasing the height of the upper jawbone, which will push up the sinus as a result. So the dentist will have enough bone material to drill into and place the dental implant.
However scary as it may sound, perforations are usually easy to patch with a resorbable collagen membrane to let the tissues heal. But in fact, all depends on the size of sinus perforation. With small perforations, the membrane can usually heal on its own. So don’t worry.
– Bone fracture: that can happen if there is not enough bone or with low jawbone density. The dentist can break the jaw when drilling or inserting the implant. That is quite rare as this is one of the key elements the dentist will check first before accepting you as a dental implant candidate.
How to avoid these complications?
Ok I am sure, your must be scared by now. So take a deep breath and keep in mind these complications are pretty avoidable thanks to a complete assessment of your teeth and jawbone with x-rays and CT scans, that will help the dentist check the position of anything that matters.
Do I need to underline the importance of picking an experienced and skilled dental implant dentist or sugeon?
The dentist will check carefully the position of your teeth, will identify the exact location of the nerve to avoid any nerve damage, will check if there is enough bone right under the sinus and will check the density and volume of your jawbone before the operation.
As I told you, checking your teeth and jawbone, examining the x-rays or CT scans, planning and designing the proper surgical plan for ideal location and angle are the most important steps to perfect execution without complications.
Rejection of the Implant
It is very rare and somehow a subject about which all dentists don’t have the same opinion but I guess it is still worth mentionning.
You probably know that the human body has a kind of built-in protection against anything that it considers “foreign”. That is our awesome immune system whose mission is to protect your body against any potential harmful agents.
This is the reason why tissues and blood samples are thoroughly analyzed during any transplant procedure so that the donated organ will not be rejected by the body.
Here, we don’t have a living organ, but a dental implant, which is usually made up of titanium. (At least the part that is embedded in the jawbone)
A titanium implant is an inert object. As such, the possibility of it being rejected by the body is almost zero.
In very rare instances however, rejection can happen with the implant material being considered by the body as foreign.
Yet, many dentists consider rejection is not possible, in fact they consider titanium dental implants cannot be rejected as they are very biocompatible, but they do think what we call rejection is merely in fact the result of an infection or a failed bone integration.
Whatever the real cause behind it, the end result is more or less the same: a loose implant.
Implant breaking or bending
This complication was often observed in the past with the first generation implants but advances in technology, materials used, and implant design has reduced a lot the risk of implant failure. Still, this cannot be totally avoided because implants are subjected to constant pressure over a long period of time.
In fact, implants are usually made of a titanium alloy, which you know is highly compatible with your bones but it is also one of the strongest metals. That is the reason why titanium implants are mainly used to replace the original root of your missing tooth or teeth and for other medical purposes.
Yet, even titanium has its breaking point. So, yes you can certainly break or bend a titanium implant root but that would only be possible with a huge pressure that would get you many other injuries at the same time.
But in reality, it is less and less the case. In fact, you could probably be hit in the mouth and all your other teeth would break off, except that dental implant.
In fact, most implant breaking or bending are due to a weak point: the abutment screw.
It connects the dental crown with the dental implant itself. It is a small piece that is pretty vulnerable to forces, which can break it or bend it. The good news is that part is an easy fix.
We talked about the post (the implant screw part), the abutment, but we also have the dental crown. It is the part that is the most exposed and the most visible. They are not as strong as the titanium implant itself but they are much more resistant thanks to the major advances in ceramic technology. Dental crowns are also very important and must be carefully designed for patients with heavy bites.
So yes you can break a dental implant or bend it. Excessive and continuous teeth grinding can result to implant failure (abutment breaking or bending or crown breaking or chipping) as much as a sudden blow to the face.
Allergic reaction
This rarely happens, but people with adverse reaction to titanium alloy may experience allergy or inflammation.
Patients with an oral titanium allergy would get different symptoms like burning or tingling sensation, swelling, oral dryness or loss of taste.
The thing is titanium is now almost everywhere from food to medicine.
You can find titanium dioxyde in the coating of some candies (M&M for example), in some toothpaste, and even cosmetics because it makes candy look brighter, makes the toothpaste look whiter and it can also help block UV rays from the sun in cosmetics. Mind you, this is only the tip of the iceberg…. The list is much longer….
Anyway, to determine your body’s reaction to titanium, you may need to undergo a MELISA test—the only know scientific procedure known to detect allergy or sensitivity to metals. (Aka Memory Lymphocyte Immuno Stimulation Assay)
Yet, keep in mind titanium is not always the culprit because some titanium alloys contains traces of nickel and other metals such as vanadium, aluminium are also added to improve the properties of titanium implants.
So if an allergy is supected, you should try to find out the exact composition of the implant and then you would have to test any allergy to the other metals as well.
If you are really allergic to titanium, does it mean you can’t have dental implants?
You still can because you can get zirconia dental implants, which are the best solutions for patients looking for metal free implants.
The reasons why dental implant may not be the best option for you
So aside from the risk involved (although very minimal) of the surgery, there are instances when a dentist might refuse to perform dental implant operation on you to avoid those dental implant problems.
These reasons include:
- Inability to find the location of the lower jaw’s primary nerve which might result to nerve damage
- Insufficient jawbone dimension and density that cannot be corrected by bone grafting
- Uncontrolled diabetes
- Use of intravenous or oral bisphosphonates (fosamax, actonel and boniva) – medicine used to prevent osteoporosis or cure other bone-related ailments. (long time treatment)
- Severe or chronic clenching or grinding of teeth (also called bruxism)
- Smoking
If you were brave enough and patient enough to read the whole post, then I guess you may think implants are not for you. Even though you seem to present several contraindications, that doesn’t mean you can’t be a good candidate for implants.
As I told you earlier, dentists need to see the whole picture of your medical and dental history. It is like adding up all the pros and cons.
Besides, with constant advances in dental technology, they may be able to find ways to safely place implants even though it was not possible a year ago.
Yet, you would need to consult an experienced and skilled dentist and that must be your first concern.